Cervical disc herniations present with symptoms that are analogous to those produced in the lumbar spine. MRI studies of asymptomatic individuals indicate that 40% of patients studied have disc abnormalities. Pain radiating down the arm is a hallmark of an acute disc herniation in the cervical spine. Because of the presence of the spinal cord, severe disc herniations can cause spinal cord dysfunction, which include weakness in the legs and balance problems. Generally speaking though, the presentation and duration of symptoms in the cervical spine is similar to that of the lumbar spine. 60-80% of acute symptoms will resolve in 4-6 weeks with rest and other conservative measures.
During this time, the spine should not be manipulated in any way. Muscle and sensory weakness or abnormality can be increased with any manipulation except longitudinal traction applied gently on the neck bones. Medications such as anti-inflammatories or a short course of low dose steroids can reduce the inflammation until the natural history of the problem until complete resolution occurs.
For patients who remain symptomatic beyond 6-8 weeks of conservative care a decision about interventional treatment should be discussed between the patient and the physician. Increasing pain is a relative indication for surgery on the cervical spine. Muscle weakness or sensory changes which continue for 8-12 weeks or progressive neurological deficit are strong indications for surgical intervention. Signs of spinal cord compression such as balance or bowel and bladder problems are another strong indication for aggressive intervention.
Unlike the lumbar spine, simple cervical discectomy is rarely indicated. Cervical disc fragments which are completely detached and presenting in a far posterior lateral position, may be amenable to removal by posterior techniques without fusion. Most cervical disc herniations are best treated with an anterior neck approach, removal of the disc fragments in the spinal canal coupled with an anterior interbody fusion with either the patients bone or bank bone. The decision to place plates and screws should be individualized for each patient.
The artificial cervical disc may be an option for certain patients. The Prestige Artificial Disc was approved by the FDA in July, 2007. The Bryan Artificial Disc was approved by the FDA on May 12th, 2009.
The approach to the anterior neck makes use of a plane between muscles, which is very easy to recover from. The muscles naturally part, allowing the surgeon direct access to the spine. The approach is made thru a small incision approximately two inches in length. The incision is carefully made in the natural lines of the skin to minimize scaring. In the majority of patients, the scar is not noticable after the initial recovery period.
If done correctly, a single level anterior cervical discectomy and fusion might be accompanied by 24-48 hour maximum hospital stay.
For single level fusions, the use of the patient’s own bone versus bone from a bone bank yields similar results. Although the use of a plate and screws for a single level fusion may reduce the postoperative need for a cervical collar, the ultimate result with or without a plate is probably similar.
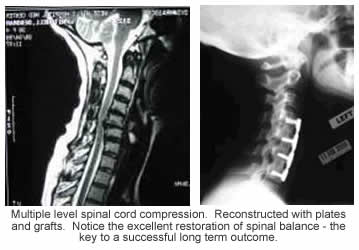
If the fusion includes more than one level, the use of the patient’s own bone as well as the use of a plate independently improves both symptomatic and surgical outcome. If the cervical discectomy is done with technical proficiency, the choice between different manufacturer’s plate systems is inconsequential from a mechanical standpoint. The reconstruction of a single level fusion should never rely on the plate screw system. The bone grafts should be placed with sufficient compression, that the plates and screws only act as a neutralization device, much in a similar fashion as a cast neutralizing a broken forearm bone. Plates manufactured to current standards yield little differences in outcome despite plate thickness, screw types, and screw plate interfaces. A surgeon selling a neck surgery wholly based on a particular manufacturer’s plate-screw combination should be viewed with abject suspicion.
It is a given that the offending compressive tissue should be adequately removed during the surgery. Soft disc herniations as well as bony ridges should all be removed if they compress nerve tissue. Aside form solid, bony fusion; one little recognized goal of any reconstruction surgery should be the creation of normal cervical lordosis. Grafts, which are misplaced or collapsed into kyphosis, may have long term negative impact on the results of the surgery over the long term.